Cognitive Behavioural Therapy (CBT) is a therapeutic approach that research has shown to be an effective treatment for anxiety and depression amongst other issues. In this article I’ll explain the basics of CBT, look at some recent developments that combine CBT with mindfulness. I’ll also offer some thoughts as to some pieces I think can be missing from a strict CBT approach.
What is CBT?
CBT stipulates that there is a strong connection between thoughts, feelings and behaviour. The way we see things and the way we think of them influences how we feel and what we do.
An example of the effect of negative thinking:
Situation:
You walk down a street and recognise a friend on the other side of the street. You wave or shout his name. He doesn’t respond.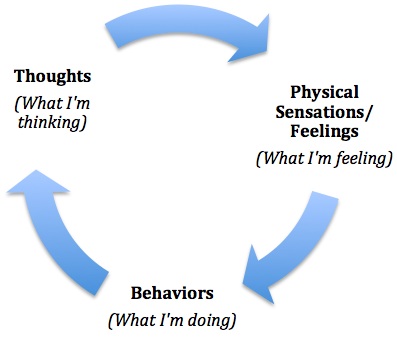
What happens?:
Person A might think: “Oh, John must be ignoring me. I wonder if it’s because of what I say the other day. I bet he’s upset with me.” Person A goes on with his day worrying, feeling anxious and distracted (mood/emotion). This affects his ability to concentrate at work (behaviour). He plans to avoid the game tonight that John is likely to be at, just to avoid more stress (behaviour).
Person B might think: “Oh, John must be distracted with something, or maybe he’s got earphones on that I can’t see. Who knows. I’ll see him at the game later anyway”. Person B goes along with his day as if nothing happened, is able to focus at work, and enjoys the game that night with John.
What does CBT therapy involve?
CBT helps you increase your self-awareness by identifying your common negative thoughts and how they influence your emotions and your behaviour. We work towards helping you intervene in any point in the thoughts-feelings-behaviour cycle to create a healthier and more positive outcome.
CBT suggests negative thinking is based on unrealistic assumptions – check out this list of 10 Cognitive Distortions: which do you do a lot of?! We would then find ways to “reality test” the negative or unrealistic thoughts to see if they are indeed true. We can do this through little experiments that you do during the week. We can try experiments with different behaviour and a different approach to your emotions, and see what happens too.
CBT is typically a structured approach with a lot of homework assignments. It is also a modality that works well in group settings.
Here are some of the ways I use CBT in my work with clients:
- Cognitive Restructuring – Challenging thinking patterns which feed anxiety and/or depression and replacing them with realistic thoughts about your situation.
- Alternative Perspectives –Learning new ways of thinking about and conceptualizing your difficulties.
- Self-Refection – Increasing your awareness with regard to your own thoughts, feelings and behaviours about your situation.
- Behavioural Techniques – Learning specific actions you can take to manage your anxiety and/or your mood. A common scenario would be learning techniques that you can apply in the moment to help reduce or eliminate panic attacks. Therapy also includes follow through with regard to your progress and making adjustments to the therapeutic plan as needed.
- Graduated Exposure – rating the situations that make you anxious, from lowest to highest. And then starting by facing the ones that make you least anxious while at the same time learning relaxation strategies.
- Relaxation Strategies to regulate your anxiety and manage your mood.
- Lifestyle Considerations – regulating your general stress level: choosing healthy outlets which relieve anxiety and boost your mood, such as exercise, sleep, emotional support, prioritizing decisions and commitments. For those that want to minimize the effects of alcohol, caffeine, smoking and other drug use, we look at these factors too.
- Homework – testing the situations that make you anxious or trigger mood changes “in the field” outside of the therapy office. I often approach homework as an “experiment” that will give you more information about your inner workings, and help you try out new approaches learnt in session.
My perspective on the limitations of CBT:
CBT on it’s own is honestly a bit dry for me. It’s too logical and linear and doesn’t bring in enough of the soul, history and depth of being human for me to rely on therapeutically, on its own. Whilst CBT can be useful to create insight and the beginnings of self-awareness, in my experience, many people who have done CBT groups need something more afterwards to create lasting change.
Some common criticisms of CBT:
- CBT assumes that if the client fixes their thinking, everything else will be okay. In reality there may be many issues at play; notably physical, social and economic challenges, histories of trauma and abuse that leave scars beyond the cognitive mind and that make it very hard to maintain healthy relationships with self and other. The “irrational thinking” patterns then are actually lodged in real-life experience and aren’t just mental contortions. The thinking patterns are in fact symptoms of something much deeper in many instances. See this article for more on CBT criticisms.
- Critics have also questioned the validity of the research that supports CBT so whole-heartedly.
- CBT is a clinical approach that focuses on sticking to the manual. This focus on the approach risks the therapeutic relationship, or at least risks not using the therapeutic relationship to it’s full extent. According to other research it’s the therapeutic relationship that has been shown to be responsible for the largest therapist-influenced part of the change process (Miller, Duncan, Hubble). In terms of approach, as long as the therapist and the client both can get behind it, it doesn’t actually matter which approach it is. This research was originally conducted by Lambert (1992) — he found that psychotherapy outcome variance is attributable to the following factors in discernible proportions:
- 40%: client and extratherapeutic factors (such as ego strength, social support, etc.)
- 30%: therapeutic relationship (such as empathy, warmth, and encouragement of risk-taking)
- 15%: expectancy and placebo effects
- 15%: techniques unique to specific therapies
What I prefer: mindfulness, embodiment and CBT
Through slowing down and noticing your reactions (e.g. during “mindfulness experiments” in session), we might arrive at a “distorted” belief that is underneath some problems. From my perspective, which differs from CBT, it’s important to give yourself an opportunity to explore and understand the history of the belief system that is causing concern. Indeed it may make a lot of sense that you have those beliefs. You then begin to get the capacity to be distinct from it. I, with others, call this the “adult” self as opposed to the “child” or “wounded” self that internalised these negative beliefs.
Using embodied awareness with CBT – a client’s sessionUsing a Focusing exercise, a client who’s presenting problem was anxiety sensed into her present-moment experience. She felt “tight” and “held” inside and she reported a “pressure” on her chest. I asked her to sense into an image or word that best named the internal feeling. The image of a fist came to her. As she stayed present with the fist, I directed her to inquire into it. She found the fist was gripping the words “anger”, “dissatisfaction” and “sadness” amongst others. Whilst she wanted the fist to let go, it was caught: there were critical voices inside that said it was not okay to have these feelings, so she was very hesitant to let the feelings out. With my guidance she found a face for the critic and held it at a distance. We then let the critic share it’s concern. “You need to be good, and being good includes not feeling ANY of those bad emotions. You are a bad girl if they are there”. (These would be core beliefs I believe in CBT language). My client was able to recognise these as being strong messages from her childhood. Beliefs that she as an adult really didn’t agree with. (“Reality testing” the thoughts/beliefs in CBT). Yet she recognised that the beliefs keep her in a state of anxiety since she is resisting what is actually true for her – that she feels a range of emotions. Throughout this, though my voice and words I invited calm kindness towards the fist and the held emotions, validating why it makes sense they are there. I helped her identify more realistic beliefs and supported her to recognise that whilst as a child these beliefs were not optional, she now has a choice an adult. To help her stay with and strengthen her adult self, I invited an inner resource my client had previously identified (imagining herself standing next to a particular tree). Through using that imagery she was able to stay with her new beliefs and the critics’ face and intensity became more distant. Towards the end of the session she could tangibly feel the difference inside – she felt more relaxed inside and the “fist” was looser. |
It’s through this kind of embodiment and mindful awareness that I believe we heal. I believe it is that healing which enables us to think and act in different ways, rather that simply dialoguing with ourselves at a logical, cerebral level.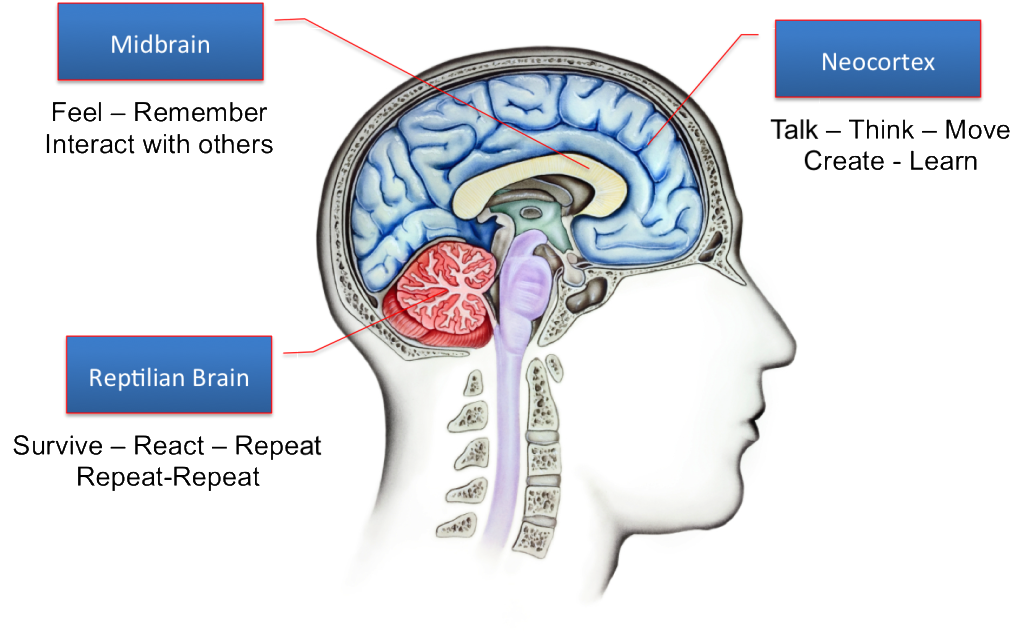
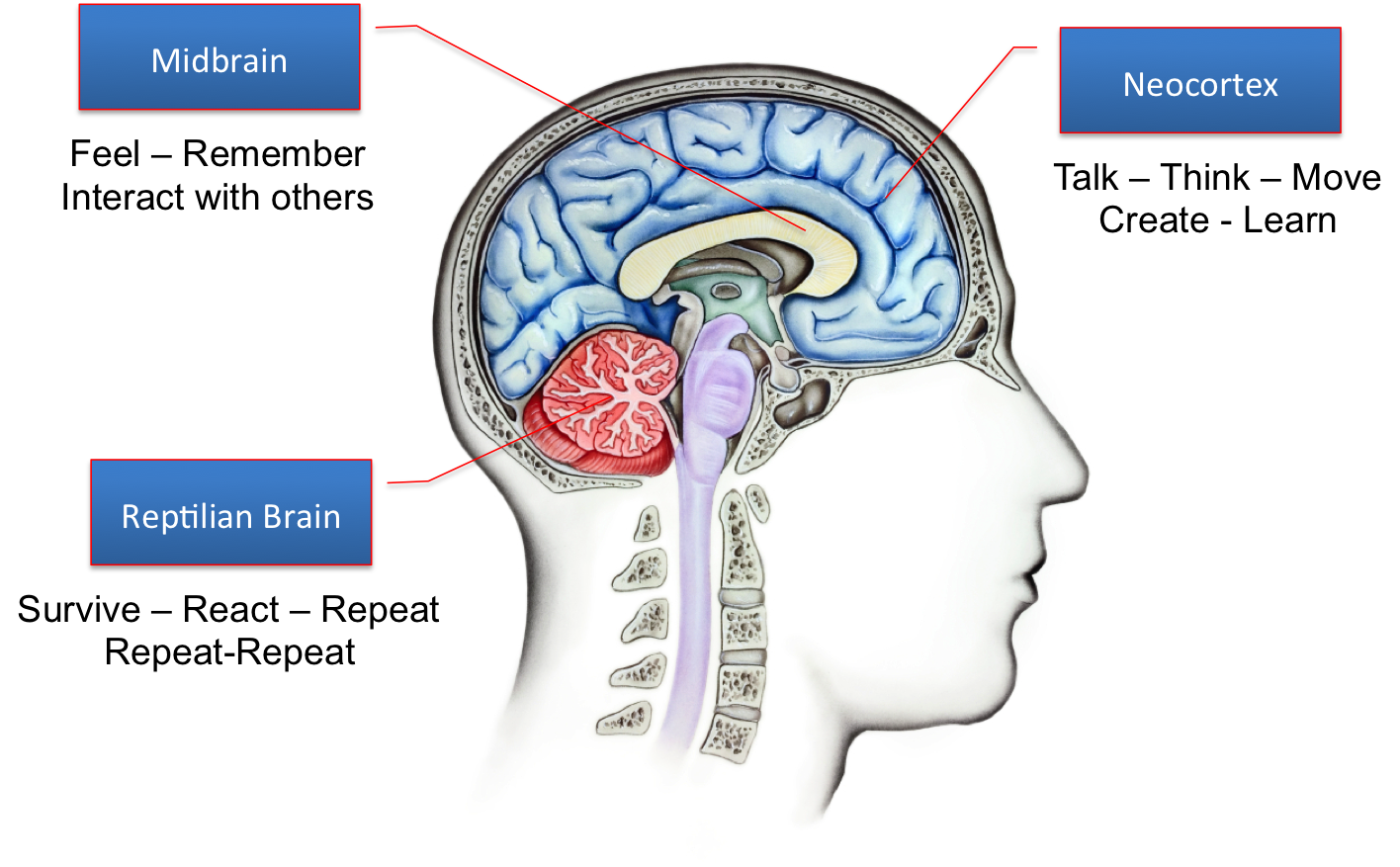
Part of why this is true is that entrenched negative beliefs are, as I understand it, linked to the limbic brain (the part of the brain where emotional memory is stored). If we are acting from an activated limbic brain, we don’t actually respond to the cerebral cortex (the thinking brain) as Dan Siegel has demonstrated (see his hand model of the brain here which explains this). So the logical self-talk of CBT risks missing the reality of the emotional/historical brain.
Notably some more recent models move in the direction of integrating neurobiology, mindfulness and CBT. Acceptance and Commitment Therapy brings kind acceptance to difficult emotions rather than just trying to ignore or get rid of them. Mindfulness-based CBT is another therapy integrating CBT with mindfulness. In addition models of CBT have been developed specifically to address trauma, and these incorporate more neurobiology and present-moment safety-creating skills which appeases some of my concern. It seems that the mainstream is also recognising the limits of CBT and moving beyond the original basics laid out by Beck and Ellis.
n.b. If you are reading this and you are a CBT practioner and want to offer your perspective and experience, and/or correct any short-sightedness shown here, by all means I welcome your input by email.